First Success in IVF Treatment
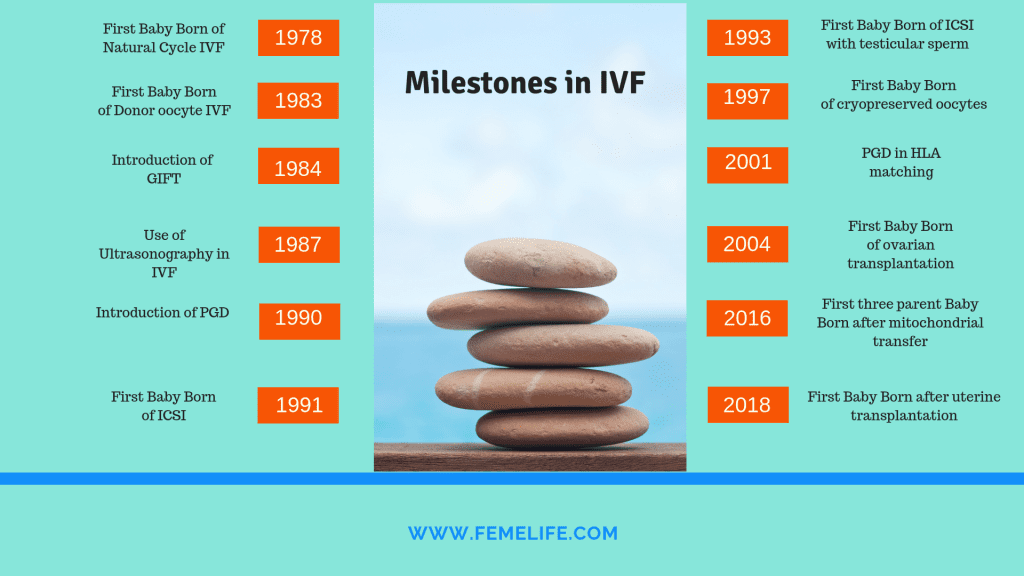
Lesley Brown was a patient with nine years of primary infertility who sought the assistance of Patrick Steptoe and Robert Edwards at the Oldham General Hospital in England in 1970’s. At that time, she was unaware of the historical revolution in IVF treatment she was going to be associated with. Fertilisation of oocytes outside the human body, a process known as in vitro fertilisation (IVF), was considered entirely experimental and unsuccessful around that period. Without using medications to stimulate her ovaries, Lesley Brown underwent laparoscopic egg retrieval, with her single egg fertilised in the laboratory, and later transferred back into the uterus. The embryo transfer resulted in the first live birth from IVF, a daughter Louise Brown, who was born in July 1978.
Introduction of ovarian stimulation and Success with traditional IVF
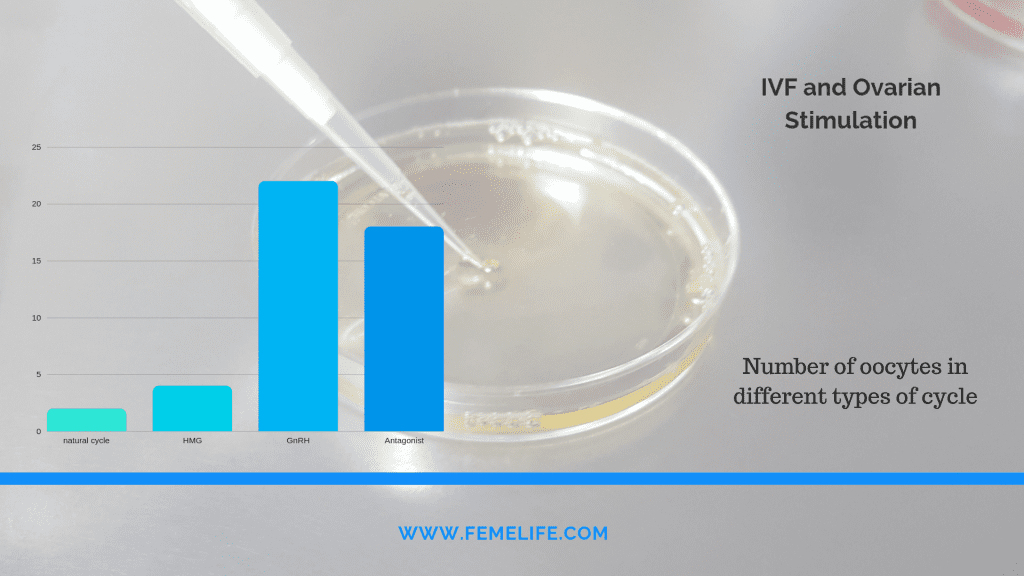
The success of IVF treatment with unstimulated cycles yielded on average 0.7 oocytes per retrieval and an overall pregnancy rate of 6% per initiated cycle at that time. Stimulated IVF cycles with human menopausal gonadotropin (hMG) prior to laparoscopic egg retrieval was extensively studied at the Jones Institute after 5 years. Its widespread use led to dramatic improvement in oocyte yield per retrieval and pregnancy rates. Between 1980 and 1983, the use of hMG with IVF treatment resulted in an average recovery of 2.1–2.6 oocytes per retrieval and increasing pregnancy rates of 23.5% per retrieval in 1982 and 30% in 1983.
Pituitary desensitisation by administration of gonadotropin releasing hormone agonist (long protocol) prior to ovarian stimulation with hMG was first reported in 1984. Effective suppression with this protocol decreased the incidence of premature ovulation to about 2% and significantly improved overall pregnancy rates with IVF.
Pregnancy rates in women using donor oocytes are known to be as high as 50% per embryo transfer in recipients across all age groups. Indeed, women in their sixties have also given birth with donor oocytes, demonstrating that the postmenopausal uterus maintains the capacity to support pregnancies if provided adequate hormonal support. Despite these unresolved issues, donor IVF remains an integral part of modern ART, and accounts for 11.6% of the IVF treatment cycles.
Freezing techniques in IVF Treatment
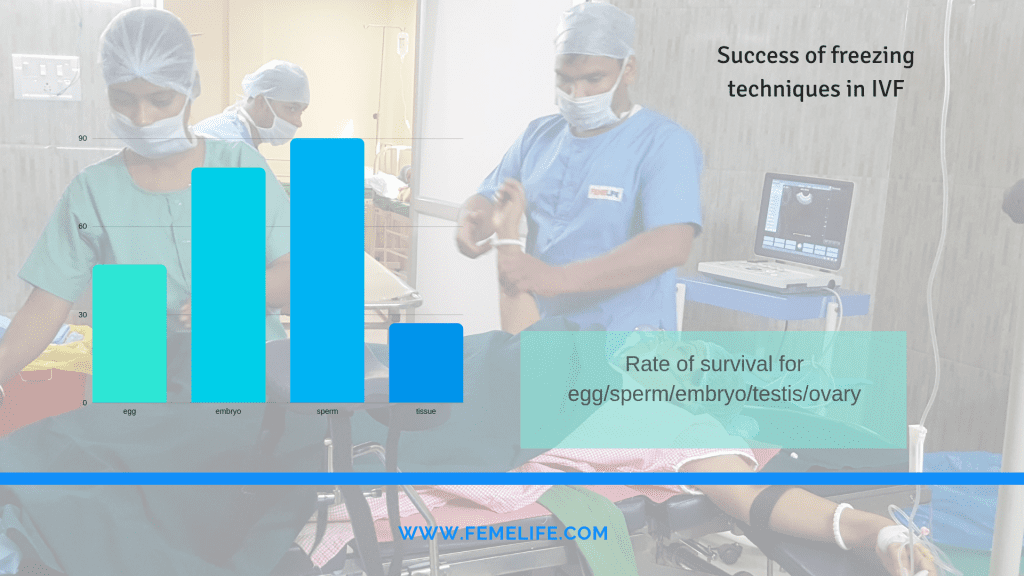
Intense efforts to develop various freezing/thawing techniques and cryoprotective agents eventually resulted in the first reported human pregnancy from a frozen embryo in 1983, which unfortunately ended in premature rupture of the membranes and termination of pregnancy at 24 weeks of gestation. Despite the initial set back, technology in cryopreservation continued to improve throughout the 1980s, leading to an increase in embryo survival rate and pregnancy rates. During the initial years of experimentation, at best approximately 50% of embryos survived the freeze/thaw process and resulted in a pregnancy rate of 13.4% per embryo transfer procedure, as only 4.6% of the individual thawed embryos implanted
ICSI revolutionised Artificial Reproductive Techniques
As the pregnancy rate of IVF improved over the last decade from 22.3% in 1995 to 33% in 2003. In 2003, GIFT and ZIFT were used in only 0.1% and 0.4% of ART cycles, while IVF represented the remaining 99.5% of cases.
The first pregnancies using embryos generated by ICSI were reported in 1992 (Palermo et al 1992) and the procedure has been applied increasingly from 11% of IVF treatment cycles in 1995 to 55.6% in 2003. Fertilisation rates as high as 70% can be achieved with testicular sperm extraction (TESE) despite only using a few poor-quality sperm. The first clinical application of the procedure called preimplantation genetic diagnosis (PGD) was used in 1990 to prevent the transmission of two X-linked conditions: adrenoleukodystrophy and X-linked mental retardation
Better Freezing success with Vitrification
Currently, each thawed oocyte has a mean survival rate of 47%, fertilisation rate of 52%, but pregnancy rate of only 1.52%. Other methods to circumvent oocyte damage caused by the freeze/thaw process include vitrification and cryopreservation of germinal vesicles. Vitrification uses high concentration of cryoprotectants to solidify the cell into a glass-like state without the formation of ice. Based on a small study, post-thaw survival rates and pregnancy rate of this approach were 68.8% and 21.4%,
Fertility Preservation is a breakthrough in IVF treatment
Ovarian tissue cryopreservation, achieved by biopsy and cryopreservation of ovarian cortex containing primordial follicles, followed by thawing and transplanting the autograft after completion of cancer treatment offers a potential solution in those circumstances. Transplantation can be either orthotopic (in close proximity to the infundibulo-pelvic ligament) or heterotopic (ie, forearm or abdomen). improving the efficiency of oocyte cryopreservation and of ovarian tissue transplantation promises to provide options to women who must delay childbearing.

