What is an ectopic pregnancy?
Ectopic pregnancy occurs when the fertilized oocyte implants at a site other than the uterus. In majority it is found in the fallopian tube but can happen at other sites like the ovary, abdomen or cervix. Moreover, this condition is a dangerous situation in a woman’s life as it can cause life threatening bleeding.
What are the risks for ectopic pregnancy?
Up to 50 % of women diagnosed with ectopic disease don’t have any risk factors. However, few of the conditions increasing the risk for ectopic gestation are:
- Previous ectopic pregnancy
- Tubal damage from infection or surgery
- History of infertility
- Therapy for in vitro fertilization
- Increased age
- Smoking
- Prior pelvic infection
- DES exposure
- IUD use
- Pregnancy conceived by assisted reproduction.
Why does tubal ectopic pregnancy occur?
Fallopian tube facilitates fertilization of egg and sperm in females. Accordingly, it is designed to carry out transport of egg and fertilized embryos. Any alteration of this normal process can arrest the migration of embryos and lead to ectopic implantation. On the other hand, this highly delicate procedure of embryo transportation depends upon the small hairy surface of tubal lining. In addition, the muscles of the fallopian tube contract and help in movement of the embryo. Also, the hairy surface of the tube has a smooth wavy movement directed by chemical signals from the embryo. Damage to the ciliary surface of fallopian tube can occur due to
- Infections
- Toxins from smoking
- Immunological causes
- Hormonal alterations
Can smoking cause ectopic pregnancy?
Smoking causes an inflammatory state in your body with release of various chemicals. These in turn alter the tubal lining promoting embryo receptivity for implantation. In addition, it decreases the movement of cilia and their number. This deciliation process along with abnormal signals produced by tobacco disrupts transport of the embryo.
Infections of the tubes
Infections from previous surgery or miscarriage can induce tubal dysfunction. For instance, an infected appendix can lead to dysfunction or blockage of the right fallopian tube. Specifically, some of the infective organisms like Chlamydia trachomatis infection can alter the signal for embryo implantation. Even any previous pelvic inflammatory disease can predispose you to EP. Such other potential infections causing tubal damage are Neisseria gonorrhoeae, Mycoplasma and schistosomiasis.
Is ectopic pregnancy more in elderly women?
Women over 35 years show more chances of ectopic gestation. It may be due to age-related tubal dysfunction and transportation or repeated interventions for infertility. Also, conception with assisted reproduction increases the risk for EP.
Recurrent ectopic
If you have a history of ectopic pregnancy then it raises the chance of a second ectopic by 10 times. This may be due to the damage added by the first ectopic pregnancy to the previous existing causes. However, some women do conceive naturally through the other healthy tube. Some other women may need fertility treatment like ovulation induction and IUI. Majority will require IVF treatment for conception.
Previous pelvic surgery
Any previous pelvic surgery increases the risk for EP; it may be tubal or surrounding tissue. Some of them are
- Tubal anastomosis after sterilization
- Salpingostomy for ectopic pregnancy
- Tuboplasty for removing blocks
- Lysis of adhesions in endometriosis or PID
- Endometriosis, appendicitis, or other pelvic surgeries, may change the anatomy of the fallopian tube
Which contraceptive can lead to ectopic gestation?
Some women using IUD do conceive and have high chances of an ectopic gestation. Other contraceptives are not associated with it. Modern IUD devices have less risk.
Is IVF a risk for ectopic pregnancy?
Risk of EP is more in women undergoing IVF treatment. This may be due to:
- The reproductive and medical characteristics of the woman
- Embryo quality and implantation potential
- A history of infertility in relation to age and duration
- Tubal factor infertility is associated with a two-fold risk of EP following IVF
Assisted reproductive technologies constitute a risk factor for EP, as 2–5 % of pregnancies from assisted reproductive technologies are ectopic.
Following are the factors contributing to this increased risk:
- Cycles triggered with gonadotropin releasing hormone (GnRH) agonists may have high risk of EP due to poor endometrial receptivity
- The more number of embryos, more the EP risk
- Transfer of embryo in mid cavity is safer than a fundal transfer
- The transfer of fresh embryos is associated with a higher EP risk than cryopreserved cycle due to hyperstimulation and hyperestrogenic environment affecting receptivity
Why is it dangerous to life?
Human embryos grow safely in the uterus of the mother till delivery. The uterus is designed to receive and nurture the embryo and also accommodate a growing fetus. In ectopic pregnancy embryo implants at a site other than the uterus where the embryo can not be nurtured or accommodated. After 5 to 6 weeks of pregnancy the site ruptures causing severe bleeding. This situation if not attended quickly can cost the life of the mother.
What is the cost of treatment for ectopic pregnancy?
Due to the ultrasound facilities ectopic pregnancies are detected early nowadays. This diagnosis is combined with your blood HCG levels. At times before the appearance of the gestation sac your doctor may suspect ectopic due to the absence of doubling of HCG. Hence serial beta HCG levels with repeated ultrasound can detect the ectopic pregnancy at an early stage. At this stage you will need medical treatment with observation. It is a safer situation for you. It will not cost you more except the hospitalization charges.
But in cases of advanced gestation women tend to report with ruptured ectopic. Since this is a life threatening situation, it will require several blood transfusions, surgical intervention and ICU care. In this situation the cost is higher and may exceed your estimation.
Do I need to sacrifice the tubes after ectopic pregnancy?
Many cases of ectopic pregnancy that are detected early can be treated with medicines. Here your tubes may be spared although later may reveal a partial or complete block. However, if you need surgical intervention your doctor will decide the type of surgery on the table. If it has not ruptured she may just remove the sac and leave it as such (Salpingostomy). Similarly, partial removal or complete removal is advised if it has ruptured and the tube has distorted anatomy (Salpingectomy).
What happens in ectopic pregnancy?
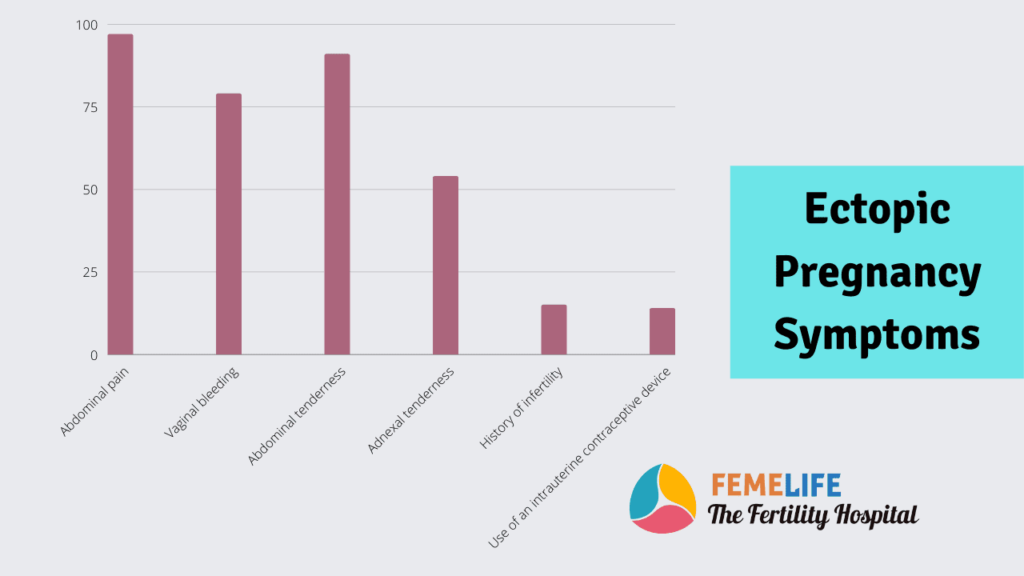
Upto seven weeks of pregnancy you may not experience any symptoms. At times women present with early pregnancy bleeding and symptoms of miscarriage. Majority present with abdominal pain which is sudden and sharp. Usually this pain occurs in one side of the lower abdomen. There is no pain in 10% cases and they may present with a heaviness. Most women with a positive pregnancy test and sharp abdominal pain are the definite cases of ectopic pregnancy. In cases of tubal rupture women present in a collapsed state.
Diagnosis
Your doctor relies on a sensitive pregnancy test and ultrasonography for the diagnosis of this condition. Absence of pregnancy inside the uterus with a positive pregnancy test will raise the suspicion. Consequently, she will advise a serum beta HCG test to confirm.
The diagnostic features of this condition are
- Absence of doubling of HCG in blood in 48hrs
- No sac in ultrasonography
- Presence of mass in USG
- Low concentration of Blood HCG
Does it affect your future pregnancy?
The major consequences of having ectopic pregnancy are
- Infertility due to damage to the tube
- Recurrent ectopic
- Rupture of uterus in cases of cornual pregnancy
- Psychological consequences or fear of pregnancy