Sonosalpingography (SSG} is a procedure primarily used to check your fallopian tubes. It is done as apart of infertility investigations. It is popular among doctors and patients because of the safe and painless procedure. Along with the evaluation of tubes the uterine cavity is also evaluated. If your doctor suspects an abnormality in your tubes or blockage of tubes, she may ask for it. Before your IUI procedure, you need to check the tubes and make sure that your tubes are healthy.
Saline sonohysterography (SIS or SHG) is a method to assess the uterus and the state of the uterine cavity. SHG utilizes ultrasound and clean saline fluid to show the uterus and endometrial (uterine coating) cavity. The reason for existing is to recognize any variations from the norm. Sonosalpingography can be combined with Saline sonohysterography and done at the same sitting. As a result, we can check the fallopian tube and the uterus at the same time.
For what reason is Sonosalpingography performed?
SSG is required to see the patency and functioning of fallopian tubes. Any blockage of tubes or abnormalities of tube movement can be detected. SHG can likewise be performed to see the structure of the uterus. This might be done in ladies with intrinsic variations from the norm of the uterus. For example, women with repetitive premature delivery may have problems within the uterine cavity. Polyps or suspected scar tissue inside the uterus can also be found out. SHG may likewise help confirm uterine irregularities discovered during a standard ultrasound.
Why SSG is better than routine ultrasound?
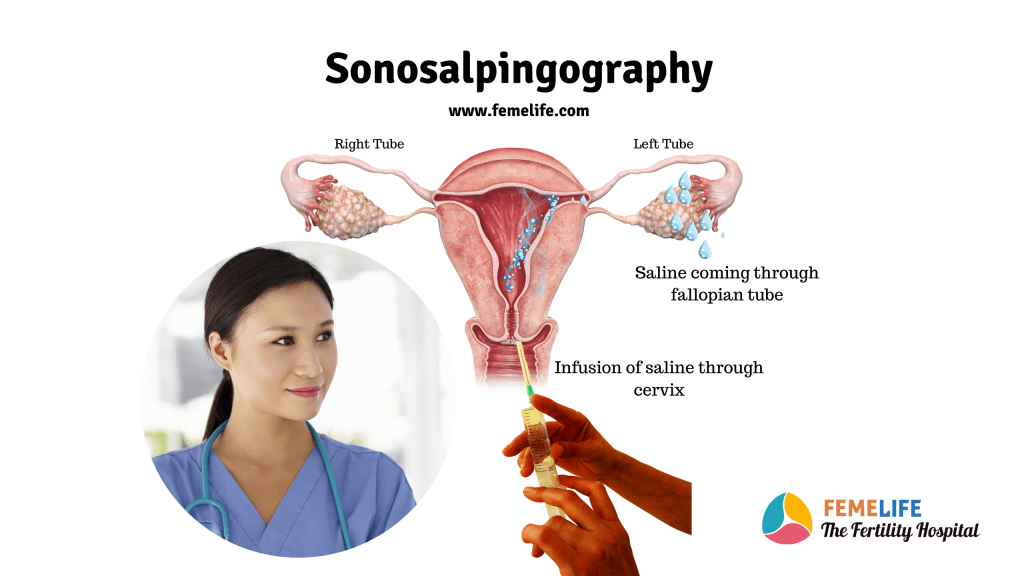
While transvaginal ultrasound is done for assessment of uterus and ovaries, normal fallopian tubes cannot be visualized. This is so because there is no tissue-fluid interface between the tubes and surrounding. Fallopian tubes can be identified only when there is fluid in the tubal lumen or outside the tubes. This means that tubes can be identified on ultrasound when either there is hydrosalpinx or free fluid in pelvis or fluid is introduced in the tubal lumen or in the pelvis. Fluid can be introduced using a catheter through cervix to visualize and assess the fallopian tubes by ultrasound.
When is SSG/ SHG performed?
SHG is generally done after the menstrual period or flow stops. In ladies who are not having a regular cycle like those on medications, it might be done whenever. For postmenopausal women, SSG is not required as they are not ovulating but SHG may be indicated to see any problem in uterus. In these situations, it is carried out after a withdrawal bleeding is achieved following the administration of progesterone tablets. This is to ensure that the test is done when the endometrium was thinnest and also to exclude early pregnancy. The method starts with an ultrasound done through vagina {transvaginal ultrasound}. Women can go through this procedure while bleeding also. But saline infusion sonohysterography or Sonosalpingography is avoided whenever possible, as the blood clot may show as a tumor inside.
How a woman is prepared for Sonosalpingography?
Sonosalpingography is ideally done in the mid-cycle of menstruation (day 6-10 of a typical 28-day cycle). Preferable after menstruation stops but before ovulation occurs. This is done to reduce the risk of disturbing an early pregnancy. Oral painkiller medication may be given 1-2 h before the procedure. This is given to avoid mild cramping pain felt in some women. You will be checked for infections like chlamydia and an oral antibiotic may be prescribed to prevent infection during this procedure. This process has to be done in a sterile environment. Your doctor will make sure that you don’t catch any infection.
A transvaginal ultrasound scan will be done to see the position of the uterus or any signs of pregnancy. Additionally, she may ask for a urine pregnancy test if any suspicion of pregnancy arises. Your specialist will make sure that there is no problem during this test. Moreover, any free fluid in the pelvis is also checked to rule out infection.
Counselling
Preparation for the examination involves counselling of the couple. Your doctor will explain about the procedure and obtain an informed consent from both of you. The instruments used for the procedure are a sterile speculum with an open side and uterine sounds in the event that the catheter did not pass easily through the cervix. In addition, the procedure tray will contain a 20-mL syringe, a tenaculum, and a soft catheter though which the saline will be injected into the endometrial cavity. The average duration of the procedure is 5 minutes with a range of 4-9 minutes.
What is the procedure of SSG?
You will be placed in usual gynaecological examination position. After cleaning and draping your doctor will introduce a sterile speculum in the vagina. With this she will be able to see the whole of cervix and its mouth {os}. The cervix is then cleansed with antiseptic solution. Now she will introduce a soft plastic catheter through the cervical os. This catheter if passes the cervix smoothly then further advanced into the endometrial cavity.
At this point she will remove the speculum which will make you feel comfortable. Then the transvaginal probe will be put beside the catheter. Under transvaginal sonographic guidance she will push around 10 to 30 ml of warm sterile saline. This makes you visualize the inside of uterus at first followed by the left and the right tube. The catheter is then removed and the procedure completed. You will be asked to continue the antibiotics for a further period of 3-5 days along with pain killer if necessary.
What we can find out in SSG/ SHG?
When the saline is injected through the catheter slowly your uterus first fills up with fluid. This is seen in the ultrasound monitor as a dark coloured space. If your uterine cavity is fine this space looks regular. It shows irregularities in cases of fibroids, polyps, or scar tissue inside the uterus.
Scanning continues with simultaneous injection of fluid through the catheter. Now this saline overfills the uterus and flows towards the tubes. At this moment your doctor can see the fluid passing though tubes and spilling around the ovary. Absence of spill may indicate blockage of the tube of respective side. It is not always possible to see the spill from the tubal end of individual tube. In such cases fluid accumulation behind the uterus confirms at least one fallopian tube is healthy and patent. In patients both side blockage, it may cause severe pain as the fluid accumulates in uterus. The specialist cannot see any spill in both sides or in the pelvis.
When SSG should not be done?
- SHG ought not be acted in ladies who are pregnant or who are suspected to be pregnant.
- SHG ought to likewise not be acted in ladies with a pelvic contamination or inflammation.
- Should be avoided in patients having any co-morbidities such as pelvic inflammatory disease, previous ectopic pregnancies or endometriosis.
- During periods of heavy bleeding
- Any suspicion of cancer of cervix or uterus
What is the cost of Sonosalpingography {SSG}?
The usual pelvic ultrasound in most of the clinics ranges from 1000 to 2000 INR. Your clinic may charge an additional 1000 INR for the Sonosalpingography. Since you have to take a course of antibiotics it may cost another 500 INR. In total this test will cost you around 3000 to 4000 INR which may vary between clinics. Along with the procedure cost you may have to spend on observation after procedure and consultation for interpretation of results.
| Consultation Medications Procedure | SSG or Saline sonography is a cost-effective procedure. You may have to spend 3000 to 4000 INR at most. Since it rarely causes any side effects it is safe to go with it. |
What are the other methods to check the tubes?
Fallopian tubes are important to carry the sperm, egg and embryo. Tubal factor is the cause of infertility in around one fourth of cases. So, checking the tubes are included in the infertility investigations.
Hysterosalpingography (HSG) is an age-old method of evaluating tubal health. It is used to evaluate the uterine cavity and the tubal status by an Xray. It uses iodinated contrast and is painful and uncomfortable for patient.
Ultrasonography – Ultrasound is used by gynecologists for the assessment of uterus and ovaries. It cannot check the fallopian tube due to lack of contrast fluid. This fluid can be created artificially by introducing saline in the uterine cavity and fallopian tubes and scanning simultaneously. The procedure is named Saline infusion HSG or Sonosalpingography{SSG}.
HyCoSy – In this method contrast agents are used for tubal assessment along with ultrasound. This procedure is known as hystero-contrast sonography (HyCoSy). Actually, it shows the flow of the contrast through tube and locates the site of block. Results of HyCoSy are as good as laparoscopic findings.
Laparoscopy – Laparoscopy is considered to be the gold standard for tubal evaluation, but is an operative procedure and needs anaesthesia. It is a costly procedure and carries all the risks of anaesthesia and bleeding, damage to the organs.
Sonosalpingography vs HSG – Which is better?
HSG is widely used for tubal evaluation as it provides optimal delineation of the fallopian tubes. It allows detection of tubal patency, tubal occlusion, tubal irregularity and peri tubal disease. In general, HSG is done in the proliferative phase of the cycle in order to ensure that woman is not pregnant when the procedure is performed. HSG allows to study the endometrial cavity in addition to its main use to assess the whole tube. The main disadvantages are –
- But the radiopaque contrast used for the procedure, contains iodine and therefore has a risk of causing a reaction.
- The procedure has to be done in the radiology set up where risk of radiation hazards are common.
- The main disadvantages are exposure to radiation and its high false negative rates.
In contrast Saline sonography or SSG can be done in an outpatient setup. It doesn’t use any contrast and there is no risk of radiation. This procedure is relatively safe and pain free. It is quick to perform and real time detection of uterine abnormalities is superior.
What are the dangers and complexities of SSG?
Sonosalpingography is an extremely safe procedure and ordinarily is performed without any mishap. The most well-known problem with SHG is pelvic contamination. But the rate of infection is much below 1% of cases. Usually post procedure infection can be avoided by proper evaluation and selection of cases. Also, your doctor may suggest intake of antibiotic before procedure to prevent such hazard.
SHG may sometimes cause mild pain, spotting, and vaginal bleeding. A few ladies continue to have pain for a few hours after procedure is over. It is avoided by taking the prescribed medicine. You should call your primary care physician in the event that you experience any discomfort or fever in the 1–2 days after the SHG.
Saline infusion sonohysterography is a safe, cost effective tool in the evaluation of the uterine cavity prior to IVF treatment.
What are the other advantages of SSG?
Saline infusion sonohysterography is also used to evaluate the uterine cavity prior to IVF treatment. Intra-uterine lesions play an important role in the outcome of assisted conception procedures. It can detect abnormalities like
- Submucous fibroids accounted for almost half (48.57%)
- adhesions (28.57%)
- endometrial polyps (22.86%)
- Small uterine cavity
- Adenomyoma
- Polypoid endometrium
Saline infusion sonohysterography is a cost-effective and dependable method. It is a safe diagnostic test in the evaluation of the uterine cavity and tubes before fertility treatment. With minor side effects, it is better tolerated by patients. It can assess the tube and uterine cavity at the same time. It is patient friendly due to the cost factor and also encourages your doctor as it is less risky.