Thick Endometrium
Thick endometrium or endometrial hyperplasia is a condition where the uterus lining causes heavy or abnormal bleeding. This can expose you to the risk of endometrial cancer or uterine cancer. Thick endometrium usually occurs during or after the menopause. Progestin therapy helps to relieve the symptoms. Women who are at risk for cancer may choose to get a hysterectomy. Endometrial hyperplasia is also a fertility issue in the female reproductive system. The lining of the uterus is known as endometrium which becomes unusually thick because of having too many cells (hyperplasia). Infertility, miscarriages and implantation failure are some of the fertility issues with thick endometrium.
How common is thick endometrium?
Endometrial hyperplasia is a rare case. It affects approximately 130 out of 100000 women’s. But some women are at risk of developing thick endometrium on hormone therapy. Diabetes, high blood presure and thyroid diseases can increase endometrial thickness.
Who might have endometrial hyperplasia?
Women who are peri-menopausal or menopausal are more usually to have the endometrial hyperplasia. It may sometimes occurs in women younger than 35 years. Other risk factors include:
- Certain breast cancer treatments
- Diabetes
- Early onset of menstruation or late menopause
- Ovarian, uterine or colon cancer in the family members
- Gallbladder disease
- Hormonal therapy
- Never being pregnant
- Obesity
- Polycystic ovary syndrome (PCOS)
- Smoking
- Thyroid disease
- White race
- Long period of absent or scanty menstruation
What are the types of thick endometrium?
The endometrial hyperplasia is described as based on the kinds of cell changes in the endometrial lining. The types of endometrial hyperplasia include:
Simple endometrial hyperplasia (without atypia):
This type of endometrial hyperplasia has very normal looking cells that aren’t likely to become cancerous. This condition will also improve without treatment. Hormone therapy will helps in some cases.
Simple or complex atypical endometrial hyperplasia:
An overgrowth of abnormal cells which causes this kind of precancerous condition. Without any treatment, the risk of endometrial or uterine cancer will increase.
What causes endometrium hyperplasia?
Women who will develop the endometrial hyperplasia produce too much estrogen and not enough progesterone hormones. These female hormones play vital roles in menstruation and pregnancy. During ovulation, the estrogen hormone will thickens the endometrium, while progesterone will prepares the uterus for pregnancy. If conception doesn’t occurs, the progesterone levels will low. The progesterone drops and triggers the uterus to shed its lining as a menstrual period.
Women’s who have endometrial hyperplasia will make low level of progesterone. Consequently, the uterus doesn’t separate the endometrial lining. Instead of this the lining continues to grow and make as thicken. Additionally, in obesity elevation of estrogen levels is seen. This fat tissue can change some of the hormones to estrogen. This is the how obesity contributes to elevated circulating levels of estrogen and increase the risk of endometrial hyperplasia.
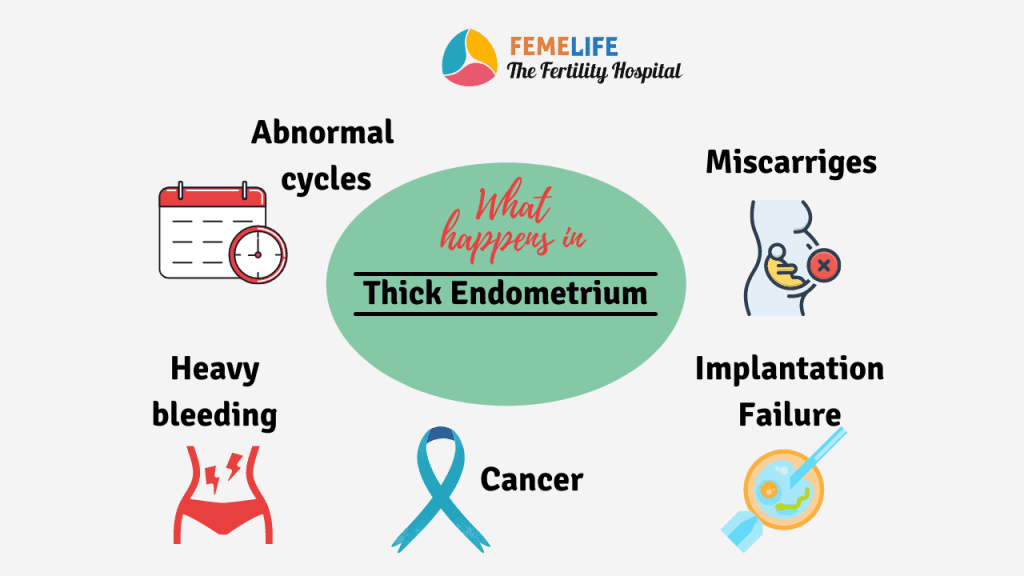
What happens when you have thick endometrium?
- Abnormal menstruation, like short menstrual cycles or unusually long periods or missed periods
- Heavy menstrual bleeding
- Bleeding after menopause
- Miscarriages
- Failure in IVF treatment
What is the relation of endometrium thickness and pregnancy?
- It has been widely suggested that a thin endometrium is related to lower IVF/ICSI pregnancy rates
- Sonographic parameters that are assessed before IVF include endometrial thickness , endometrial pattern, endometrial volume, and sub-endometrial blood flow.
- Pregnancy rate is maximum in the endometrial thickness of 8 mm to 11 mm.
- In endometrial thickness (Ent) > 14 mm, pregnancy rate is almost zero in IVF treatment cases.
| Thickness of endometrium | Cause | Effect on Pregnancy |
| Less than 6mm | Prior surgery on endometrium, Tuberculosis, Radiation therapy, hormone problems | Very low clinical pregnancy |
| 6-8 mm | Above causes, elderly age group | low implantation, ectopic pregnancy, miscarriages, IUGR |
| 8-14mm | Normal endometrium | Good clinical pregnancy |
| More than 14mm | Endometrial polyp, PCOS, Uterine anomaly | Low pregnancy with miscarriages |
How is endometrial hyperplasia diagnosed?
Many conditions will cause abnormal bleeding. To identify what’s causing symptoms, the doctors may order one or more of these tests:
Ultrasound: A transvaginal ultrasound produces images of the uterus through echo of sound waves. The images will show the lining is thick.
Biopsy: An endometrial biopsy which is test where endometrial tissues is removed and send biopsy the samples from the uterus lining. Pathologist studies the cells to confirm or rule out cancer.
Hysteroscopy: Your doctor uses a thin, lighted microscope called a hysteroscope to examine the cervix and look inside the uterus. She may combine this procedure with dilation and curettage (D&C) or biopsy. With hysteroscopy, abnormalities within the endometrial cavity can be seen. If required your doctor will take a targeted (directed) biopsy of any suspicious areas.
What are the complications of endometrial hyperplasia?
All types of hyperplasia will cause abnormal and heavy bleeding that can make anemic. Anemia develops when the body doesn’t have enough iron-rich red blood cells. Untreated atypical endometrial hyperplasia can become cancerous. Endometrial or uterine cancer will develops in about 10% of women with untreated simple atypical endometrial hyperplasia. Close to 30%of women with complex atypical endometrial hyperplasia who don’t get treatment develop cancer.
How is endometrial thickness managed?
The increased risk of cancer due to atypical endometrial hyperplasia, the healthcare provider may recommend a hysterectomy to remove the uterus. After a hysterectomy, there won’t be able to get pregnant. May peoples see symptoms improve with less invasive progestin treatments progestin comes in many forms:
- Oral progesterone therapy or progesterone hormone intrauterine device (IUD)
- Injections
Treatment:
Treatment most generally consists of hormone therapy or surgery.
The options will depend on a few factors, such as:
- If atypical cells are found
- If you have reached menopause
- Future pregnancy plans
- Personal and family history of cancer
If you have a simple hyperplasia, your doctor will suggest just keeping an eye on the situation. At times she may advise to go for any of these treatments:
Hormonally therapy:
Progestin, a synthetic form of progesterone is available in pill form and also as injection or intrauterine device.
Hysterectomy:
If you have atypical hyperplasia, removing uterus will lower the cancer risk. Having hysterectomy surgery means won’t be able to get pregnant after. It may be a good option if you have reached menopause.
How can I prevent thick endometrium?
Certain steps may reduce the chances of developing endometrial hyperplasia. Use progesterone hormone along with estrogen after menopause.
- Take the birth control pill
- Quit smoking
- Maintain a healthy weight.